
Joy Li joined Queen Mary University of London in October 2018. She is in the final year of her PhD which focuses on the screening and prevention of bowel cancer. Joy is a medical statistician by training, with 4+ years of experience in innovating the use of screening diagnostics to improve bowel cancer prevention and screening programmes in the UK. Also working on improving Breast Screening Pathways to improve access and reduce inequality. Interested in all areas of statistics, especially related to improvements towards personalised healthcare for the future.
Your PhD research is in statistics as applied to bowel cancer screening and prevention. Could you explain what you’re working on currently?
I am working on modelling the effect of using a multi-threshold Faecal Immunochemical Test (FIT) strategy in bowel cancer screening. FIT is a home-testing kit offered to individuals aged 60–74 (to be lowered to ages 50-74 by 2025). Anyone with a positive result (defined as a faecal haemoglobin level greater than or equal to 120 µg/g faeces) is recalled for further checks. This is usually a colonoscopy.
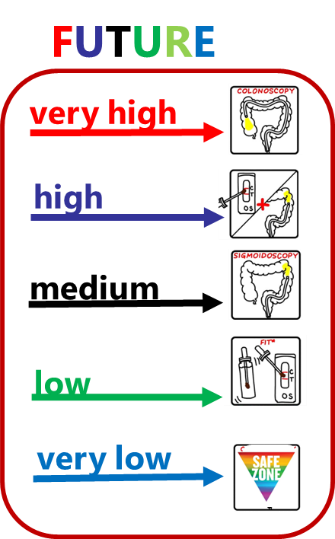
My work explores the potential of using FIT results in a more personalised and risk-based manner. Instead of a one-size-fits-all approach (a single threshold (cut-off) for referral), I estimate the different possible outcomes from incorporating multiple referral thresholds into the national bowel screening programme.
Introducing multiple referral thresholds would mean different testing and diagnostic pathways: a pathway for each respective faecal haemoglobin category. This would in turn affect overall outcomes for bowel cancer prevention, detection and early diagnosis (as well as those with high-risk and pre-cancerous abnormalities). It would also be beneficial to patients and the bowel screening programme to ensure the higher risk individuals that who would benefit the most from a further check are invited to a colonoscopy.
How did you become interested in this area of research?
Short answer: I was inspired by two amazing researchers: Professor Jane Warwick, and Professor Stephen Duffy.
Long answer: I was always interested in a career that combined Maths and Public Health (although did not know it was called Medical Statistics!). I was lucky enough to work with Professor Warwick as a research intern, on breast cancer research work, in summer 2018. The experience convinced me that cancer research was the career path I wanted to follow. I enjoyed the intellectual challenge of developing new methods and methodologies, was fascinated by the impact of the work on public health, and – most importantly – enjoyed the welcoming, friendly spirits of fellow health researchers. Fortunately, the luck continued and led me to undertake a training fellowship (NIHR) with Professor Duffy.
Professor Duffy and I started working together for my master’s thesis in the summer of 2019 (co-supervised by Professor Linda Sharples and Professor Peter Sasieni). We were looking at data from the NHS FIT pilot study conducted in 2014, which had compared FIT with the previous bowel screening test: the guaiac faecal occult blood test (gFOBT). The pilot’s result had led to FIT being introduced to the NHS Bowel Screening Programme in late 2019, as the first point of testing nationwide.
We used this pilot study data to estimate the relationship between haemoglobin concentration (measured by FIT in faecal samples) and underlying pathology of bowel screening attendees (who had a FIT result at least 20 µg/g ). Through this, we estimated the sensitivity of the FIT test (its likelihood of correctly detecting disease) of the NHS Bowel Cancer Screening Programme, in turn generated hypotheses for fuller exploitation of quantitative FIT measures.
The results were rather surprising. We estimated that, with the bowel screening programme’s existing FIT threshold (120 µg/g), just over half of all bowel cancer cases are likely to be missed. In addition, only one in four high-risk adenomas (pre-cancerous lesions) are identified.
It was clear that we simply couldn’t stop there: there was much work to be done to improve the programme’s sensitivity and overall effectiveness. Luckily, I received another studentship from Wolfson Institute of Preventive Medicine (Now, Wolfson Institute of Population Health) to continue this exploration, supervised by Professor Stephen Duffy and Professor Rhian Gabe. And have not stopped since.
More on the paper: NIHR: New Pathways Could Improve Bowel Screening Programme
What is the current screening pathway in place in England, and how does your work on FIT kit testing relate to this?
FIT is currently the first line of testing used in the NHS Bowel Cancer Screening Programme in England. FIT provides a reading of the amount of blood in a faecal sample.
Currently, only individuals whose sample found to have a high level of bleeding, at or above the threshold of 120 µg/g, receive further investigation. This is usually as a colonoscopy. As already discussed, this single cut-off (rather than multiple thresholds) may miss many bowel abnormalities. A big reason for setting the single high threshold is to manage constraints on colonoscopy capacity in the NHS. My research provides evidence on alternative screening strategies, in order to identify people with faecal bleeding below the 120 µg/g threshold yet still at risk of serious bowel issues.
Furthermore, there is plan to lower the starting age for bowel screening to 50 by 2025, meaning an increased number of people to be screened and likely additional demands on colonoscopy. Results from my work may provide evidence for strategies to minimise pressure on the health service from such increasing resource demand.
What about other diagnostic tools for bowel screening? What about outside of the UK?
There are many tools available for detecting or diagnosing bowel abnormalities. These are generally based on two diagnostic methods:
- Identifying clinical abnormalities from non-invasive biological sample, such as faecal samples or liquid biopsy (e.g. blood test) and so on. For example, FIT seeks for hidden bleeding caused by abnormalities in the bowel and rectal regions.
- Examination of medical imaging to locate the abnormalities, such as colonoscopy or CT colonography (or similar).
Colon capsule endoscopy is being tested in the NHS. This is a pill-sized device (so much less invasive than a standard colonscopy), with two very small video cameras and a wireless transmitter. These allow internal imagery of the bowel to be captured as they move through the digestive system. Colon capsule endoscopy remains new and is yet to be adopted into any national-level screening.
Most countries in Europe have a similar bowel screening programme to England. In these, FIT tests are sent to the eligible individuals at home (as the first line of testing). Any abnormal results are then usually followed up by colonoscopy or similar.
The threshold against which samples are decided to be normal or abnormal will vary, so do the eligible age for screening and the frequency for repeating the screening, by country and the healthcare resource thereof. Some countries have a slightly adapted version of England’s bowel screening programme. In Japan, two FITs are conducted over two consecutive days. And in the US, where no national screening is organised but adults of 45 to 75 are highly recommended to be screened for bowel cancer, the commonly used sampling kit looks at information on faecal bleeding in combination with any DNA changes in faecal samples.
What has your research found so far?
Results have been promising. They have suggested positive ways to improve the NHS Bowel Cancer Screening Programme. Increased colonscopy resources are estimated be required however with careful planning, hopefully these can be minimised ensuring the benefit outweighs any additional costs.
Compared with the single FIT threshold in place in England’s bowel screening programme currently, a multi-threshold FIT strategy is estimated to prevent and detect more colorectal cancers and more advanced adenomas (AA). A multi-threshold strategy requires much less FIT testing (to be published).
Early results have estimated that for every additional 2.5 colonoscopies, another advanced adenoma (high-risk tumour and potentially pre-cancerous) will be detected and removed. This has the potential to reduce the incidence of colorectal cancer.
Could these findings lead to screening programme recommendations (and updated screening pathways) any time soon? Why/why not?
I’m of course optimistic that the national screening committee will consider introducing a multi-threshold system based on our evidence plus additional evidence that is currently underway. I suspect it will be at least few years before the programme fully adopts this approach.
There are at least two more pieces of the evidence-based puzzle to complete:
- Our results are only estimates, generated from a number of statistical assumptions, meaning that another regional pilot study is beneficial. This will help to fine-tune the recommendations, for better understanding on the likely clinically impact on population of different referral thresholds, and important to recognise any operational changes required for a full-scale roll out.
- It may also be beneficial to conduct health economics research, to understand the financial and resource implications (and overall cost-benefits) in addition to overall cancer prevention and detection.
What other important research is going on alongside this?
Professor Sasieni (WIPH, QMUL), Professor Weller (University of Edinburgh) and colleagues have secured funding to explore the impact of risk-stratification in the UK Bowel Screening Programmes on a larger scale in the real-world screening setting. This is an exciting step towards making personalised screening a reality, and I am looking forward to their findings.
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorses those views or opinions.
Subscribe to our mailing list!

Leave a Reply