This post was written by Guest Authors: Alistair Thorpe, PhD and Jessica Sheringham, PhD
Positions and affiliations: Dr. Thorpe is a Research Fellow in the Department of Applied Health Research at University College London and Affiliate Fellow in the Department of Internal Medicine at the University of Utah School of Medicine. Dr. Sheringham is a Senior Research Fellow in the Department of Applied Health Research at University College London.
Drs. Thorpe and Sheringham are both part of the NIHR policy research unit for cancer awareness screening and early diagnosis, which has funded the eCREST tool and initial research into GPs’ decision making when faced with patients that might have lung cancer.
Cancer diagnosis: why do we need to look beyond GPs?

Much of the work on earlier diagnosis of cancer focuses on GPs. While GPs are of course important, primary care is changing. In England, for example, the primary care team now routinely comprises a range of professionals including pharmacists, nurses, social prescribers, and physician associates.
Physician associates (PAs) are one of the youngest clinical professional groups in the NHS. PAs are comparable to the physician assistant roles in the USA, which have existed for over 50 years. Similar roles can also be found in many other countries, including Canada, the Netherlands, and Israel. PAs are Masters level graduates who are trained for two years following a medical curriculum. Many work in hospitals, but increasingly PAs are working in primary care. Their roles vary and include seeing patients presenting with minor symptoms and management of chronic conditions. PAs cannot yet prescribe independently in the UK but statutory regulation for PAs is due in 2024. Legislation to enable prescribing responsibilities may in turn follow.
The aims of our research
From our rapid review comparing PA skills and performance relevant to cancer diagnosis, we learnt that PAs generally performed as well as physicians. This was reassuring but there was little research from the UK, where the PA profession is still new. We also learnt from this review that the successful integration of PAs, and other professionals, into primary care relies on other clinical professionals having confidence in their clinical reasoning skills.
Our research seeks to both understand and develop cancer diagnostic skills in the future primary care workforce. To do this, we have created a novel educational resource called eCREST [the Electronic Clinical Reasoning Educational Simulation Tool].
What is eCREST and how does it work?
eCREST is an online training aid for a range of clinical professionals. To date, it has been used with medical students, PAs, and pharmacy students. As primary care teams broaden, eCREST may have a role with a range of both future and current clinical professionals.
In practice, eCREST enables students to access hypothetical patient cases, via a virtual ‘waiting room’. Students can watch videos of patients describing their symptoms and review their medical history, their medications, and their lifestyle notes. The information that students obtain is determined by what options they select (e.g. through question menus, virtual ‘examinations’, or bedside tests).
At the start of each case, students are asked to select five initial diagnoses for the patient. Importantly, they are then prompted to review their initial diagnoses and are given the option to make any changes at intervals during the case.
Once the student is happy that they have enough information, they are asked to give their final selection of diagnoses, select an initial management plan for the patient, and decide on a follow-up plan for the patient.
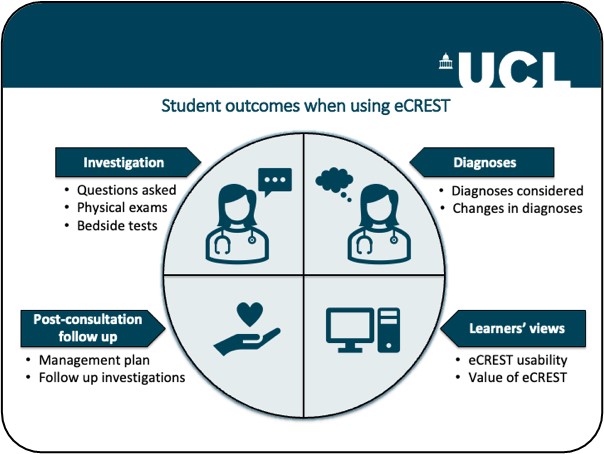
Having completed the case, students can then access tailored feedback videos by GPs, along with links to relevant clinical guidelines and further reading. Lastly, students are given the option to reflect on their reasoning and experiences during the patient case. The design of eCREST is such that there is not any single ‘right’ answer. Instead, eCREST is designed to reflect the reality of primary care patient presentations: there is a range of credible diagnoses that should be considered, identified, and acted on.
What have we found?
The results from our initial work with medical students using eCREST have been very promising. We found that medical students who used eCREST exhibited more thorough data gathering, compared with students who did not. Trial data showed that, by using eCREST, students were better able to identify the questions and tests necessary for making an informed diagnosis about the patient. Students also reported very positive experiences using eCREST.
These initial studies indicate that eCREST can help medical students practice and develop their clinical and diagnostic reasoning skills. However, from the data we had alone, it was not clear whether these findings would extend to students training for different clinical careers.
Therefore, in our latest research we are looking to compare PA and medical students’ clinical reasoning skills when faced with common respiratory symptoms that might be cancer. So far, we have recruited around 60 PA students to use eCREST, from four different UK medical schools. We are comparing their data with data previously collected from approximately 300 medical students involved in testing eCREST, from across three UK medical schools. From what we have looked at so far, the investigative and diagnostic reasoning skills of PAs and medical students using eCREST seem to be similar. However, there is still a lot more for us to investigate.
What is next?
In the immediate term, we are looking forward to attending the Health Services Research UK Annual Conference at the University of Birmingham (4th – 6th July 2023). Here we will share more details about our findings (from comparing PA and medical students’ clinical reasoning skills when faced with common but potentially cancerous respiratory symptoms).

Ultimately, we would like to see eCREST incorporated as part of the toolkit supporting clinicians to make more timely and appropriate diagnostic decisions. To reach this goal, we are seeking to expand the range of educational and professional settings in which eCREST is used. This would mean better support for future (and existing) primary care professionals in developing (and strengthening) clinical reasoning skills. We are also working with educators and clinicians to broaden the range of patient cases available to students through eCREST. For instance, we have been developing patient cases focused on bowel symptoms and testing these with pharmacy students.
We have been fortunate to collaborate with numerous medical schools to date, both within the UK and internationally, to embed eCREST as part of their curriculum. This has allowed us to work with a wide range of student groups (e.g. medical students, physician associate students, and pharmacy students) and with students from diverse backgrounds. Moving forwards with eCREST, we are always looking for new collaborations with schools who may want to use eCREST. We extend the invitation to get in touch with us if you would like to try eCREST, either as a student or an educator.
Dr. Thorpe can be reached at: alistair.thorpe@ucl.ac.uk
Dr. Sheringham can be reached at: j.sheringham@ucl.ac.uk
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.

