This post was written by Professors Freddie Hamdy and Jenny Donovan:

Freddie C. Hamdy MBChB, FRCSEd, MD, FRCSEd (Urol), MA (Oxon), FRCS, FMedSci is Nuffield Professor of Surgery, Professor of Urology and Head of the Nuffield Department of Surgical Sciences at the University of Oxford, as well as Honorary Consultant Urological Surgeon at the Oxford University Hospitals NHS Foundation Trust and Fellow of Balliol College. In 2010, he was also appointed Director of the Division of Surgery and Oncology at the Oxford University Hospitals NHS Foundation Trust. Prior to his move to Oxford in 2008, he spent 10 years as founding Chair of Urology and Director of the Division of Clinical Sciences, then Head of Oncology at the University of Sheffield. He qualified from the University of Alexandria, Egypt in 1981, and trained in Surgery and Urology at Liverpool, Sheffield and Newcastle
Professor Hamdy is Chief Investigator of the ProtectT trial.

Jenny L. Donovan PhD, FMedSci, FFPH, NIHR SI, AcSS, OBE is Professor of Social Medicine at the University of Bristol, UK. A social scientist by training, she is co-PI of the ProtecT randomised trial evaluating active monitoring, surgery, and radiotherapy for clinically localised prostate cancer. The ProtecT trial published primary median 10-year clinical and six-year patient-reported outcomes in the NEJM in 2016. The findings were included in treatment guidelines around the world. She is co-PI of the CAP prostate cancer screening trial, which published median 10-year outcomes in JAMA in 2018. Professor Donovan also leads a programme of research aiming to optimise recruitment to randomised trials and ensure well-informed participatory consent (the QuinteT Recruitment Intervention (QRI), now implemented in over 70 randomised trials in the UK, USA, and Europe.
Localised prostate cancer: does early detection and radical treatment prevent deaths?
Prostate cancer is the most common malignancy in men in the UK, with around 52,300 new cases found each year, and approximately 12,000 men dying of the disease. Despite considerable enthusiasm by some to introduce population screening for prostate cancer, there is currently no early detection programme in place in the NHS. Prostate cancer diagnosis is instead made largely through opportunistic screening.
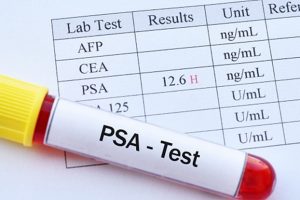
Opportunistic screening entails a blood test known as a PSA test (measuring Prostate Specific Antigen), followed by imaging using multiparametric MRI and biopsies of the prostate as indicated. This inevitably leads to over-detection and overtreatment of cancers which are unlikely to cause harm during a man’s lifetime, while underestimating the lethal potential of some tumours. The controversy about the introduction of screening for prostate cancer, and the uncertainties about the effectiveness of radical treatment, continue to be a dilemma for the NHS and other health care providers globally.
Our recently published ProtecT (Prostate testing for cancer and Treatment) study evaluated the effectiveness of treatments in screen-detected prostate cancer, following up men over a period of 15 years following study randomisation. The findings show very high survival among men with clinically localised disease (97% after 15 years), irrespective of whether they received surgery, radiotherapy, or active monitoring. Findings also show increased risks of cancer spread with active monitoring, and side-effects resulting from radical treatments.
The ProtecT (Prostate testing for cancer and Treatment) study
ProtecT is the largest randomised trial of treatment in screen-detected localised prostate cancer. It is funded by the National Institute for Health and Care Research in the UK. The trial compares:
- Active monitoring
- A form of active surveillance in which men receive regular checks and further investigations, with change to radical treatment as necessary.
- Surgery
- Radical prostatectomy, to remove the prostate gland
- Radiotherapy
- External beam radiotherapy, with a period of hormone treatment beforehand
In parallel, the quality of life of these men was investigated. This was measured through patient-reported outcomes included in an annual study questionnaire completed for at least 12 years.
The ProtecT study began in 1999 and recruitment was completed in 2009. The study began by testing 82,429 men between the ages of 50 and 69 years, across nine UK centres. Testing entailed a PSA blood test, followed by biopsies of the prostate if the PSA level was elevated.
2,664 men with clinically localised prostate cancer were found. From these, 1,643 (62%) agreed to be randomised to one of the three study treatment options. The primary endpoint was death from prostate cancer, with secondary endpoints including death from any cause, disease progression and spread, and side-effects of the treatments.
The men were carefully followed up for an average of 15 years.

So what did we find?
Men with prostate cancer lived a very long time. Only 3% died from prostate cancer, and there were no differences between men allocated to surgery, radiotherapy, or active monitoring (the three study treatment groups). Metastases developed in twice as many men under active monitoring compared with those who had radical treatment. However, this incidence was low: 9.4% compared with 4.8%.
The development of metastases in men whose disease progressed did not necessarily mean that they would die of prostate cancer. Many men developing metastases, particularly in the active monitoring group, survived up to 20 years after the diagnosis. In addition, at the 15-year follow-up point a quarter of men allocated to active monitoring had not received any treatment and remained alive and well.

This is remarkable and reassuring, even more so because a comprehensive re-evaluation of the baseline risk-stratification of the cohort indicated that two thirds had low-risk prostate cancer and one third had intermediate-risk disease at diagnosis. The situation is very different for those who present with advanced disease which has grown outside the prostate, or high-risk cancers which need urgent treatment.
Patient-reported outcomes
The patient-reported outcomes showed that, while overall health-related quality of life was similar in all treatment groups, each caused a different profile of functional side-effects. Among men allocated to surgery, side-effects included leakage of urine and difficulties with sexual function (having an erection for intercourse). These side-effects were more pronounced in this group compared with those receiving active monitoring or radiotherapy. Side-effects continued to affect some men 12 years after treatment, with some additional urinary and bowel problems emerging in the radiotherapy group in the longer term.
While the treatments given in ProtecT study used traditional techniques of open surgery and external beam radiotherapy, other studies have shown that more modern techniques – such as robot-assisted surgery and newer forms of radiotherapy – have similar side-effects. This means that ProtecT’s results remain relevant for today’s patients.
The ’good news’ story
All these findings represent good news for men diagnosed with low- or intermediate-risk localised prostate cancer. Regardless of the treatment option they choose, they will live a long time. Men now have clear information from our study to carefully assess the trade-offs between the benefits and harms of different treatment options. They are able to make prudent and well-informed treatment decisions with their doctor, partner and family, based on their own values and priorities. And they do not need to rush to make those decisions.

We think it is important to continue to follow up these men in the long term, for at least 20 years after the diagnosis. More critically, we need to conduct more research to try to understand the biological and genetic features in individual cancers which allow the disease to cause harm.
Under current UK NHS directives regarding prostate cancer pathway timelines, newly diagnosed patients with low- or intermediate-risk disease are required to make rapid decisions about their treatment. We believe these timeframes need to be relaxed. Rushing into decisions where there is no urgency and no known impact on outcomes can cause unnecessary harm and later regret. Men need to be well-informed, of both the consequences of PSA testing and the diagnosis of localised prostate cancer. Patients should be afforded time to decide, and the ProtecT study provides the relevant information they require for this.
Implications for practice
The ProtecT findings show that careful consideration of treatment options by patients is both necessary and important. Practice and policy should be updated accordingly:
- Men with clinically localised prostate cancer should be made aware of the findings from ProtecT, so that they can better weigh up the benefits and harms of treatments.
- Discussion of active surveillance as a treatment option with clinicians is highly important. This applies to men with low-risk prostate cancer, and also men with intermediate-risk, clinically localised prostate cancer.
- The short, urgent window of time between a diagnosis of low- or intermediate-risk prostate cancer and a treatment decision should be reconsidered. Men need time to carefully consider their options.
- The long-term nature of treatment side-effects needs to be understood in more detail: some effects persist, or worsen, over 12 years.
- Research efforts should now focus on identifying features which characterise lethal prostate cancer. This will enable treatment to be targeted to individual patients at risk of dying from this widespread malignancy.
Further Reading
Wall St Journal – Men With Prostate Cancer Can Thrive for Years With Less Aggressive Treatment
The Times – Why I’ve never had a PSA test to check for prostate cancer
New York Times – Debating the Value of PSA Prostate Screening
Harvard Health – Time to rethink the debate on PSA testing
EMJ Reviews – The Debate on Prostate Cancer Screening: What Does the Wisdom from the Old Books Whisper?
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.

