This blog was written by Mairéad Lyons. Mairéad is a Senior Consultant to YouScreen the HPV Self-Sampling study. She has been working in healthcare for over 30 years, first as a nurse, then in health promotion before moving into public policy research and service improvement. For the last ten years she has worked to improve patient outcomes through earlier diagnosis and standardisation of cancer service provision in Ireland and England.
♫ “YouScreen, I screen, every woman should get screened, oh yeah cervical cancer, we got you now.” ♫
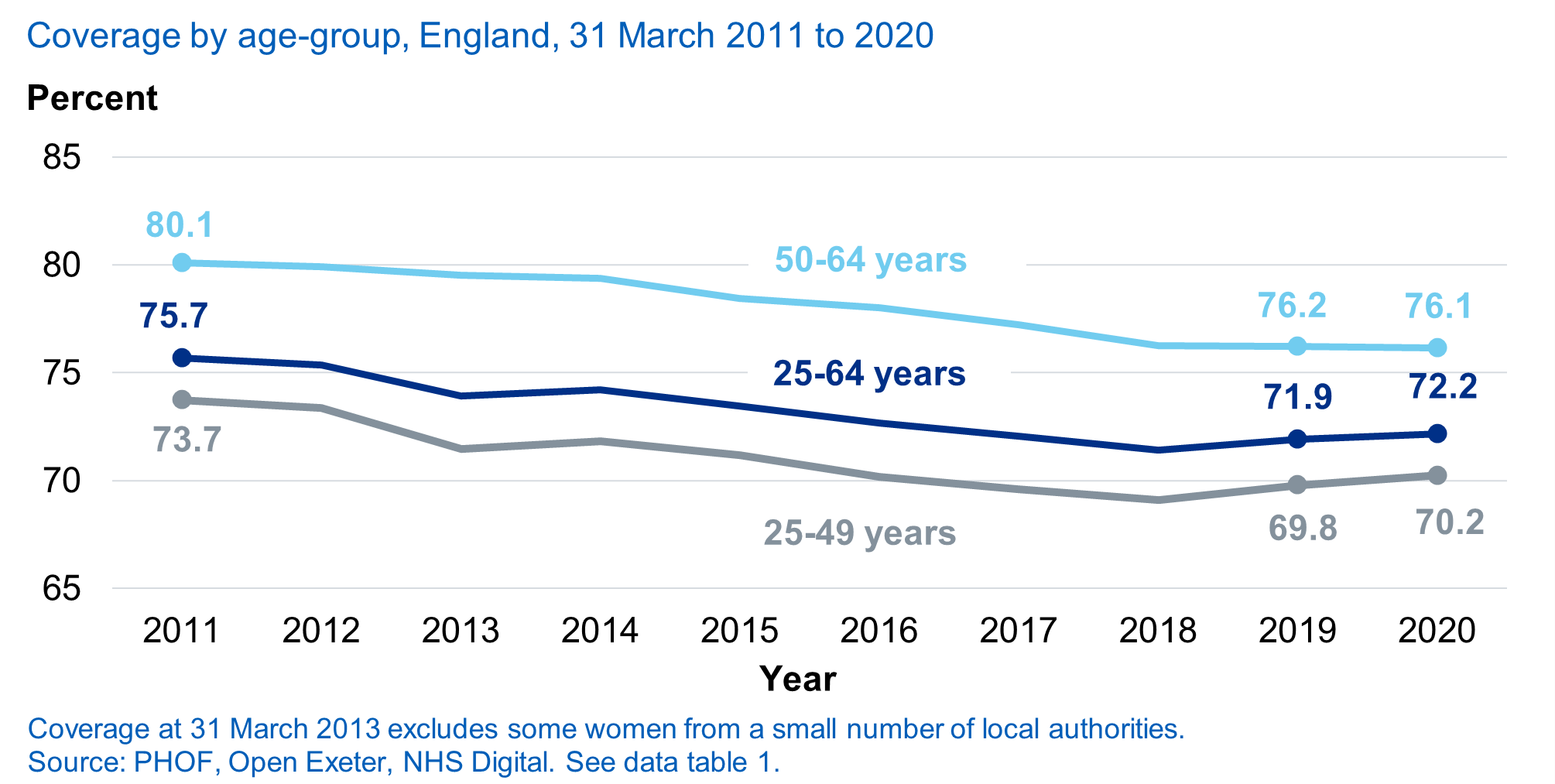
That’s how joyful I feel to finally see the YouScreen Self-Sampling Clinical Trial get underway in January this year. The YouScreen trial is a landmark study for cervical screening, as the first time self-sampling has been embedded within the NHS cervical screening programme. The trial is looking to make cervical screening easier for women and to understand more about how to implement self-sampling at scale in England. It aims to demonstrate (and quantify) that self-sampling can improve cervical screening coverage in London and can increase detection of and treatment for CIN2+. We know that screening attendance in London is consistently the lowest in England and well below the national average. In one borough in the study, as few as 55% of women were up to date with their screening in 2018/19. This is despite the many years of incentives to GP practices, cervical screening awareness campaigns and investment in innovative research projects to improve uptake and coverage. A recent study by Imperial College London in Northwest London demonstrated that the introduction of text message reminders increased cervical screening participation by almost 5%. In comparison, a recent meta-analysis suggests self-sampling can increase participation of under-screened women by 19%.
Something needs to change and we believe self-sampling is the game-changer.
Now as a woman who feels every year of my 57 years, I have had a wide range of experiences with cervical screening in four different countries, not all good. As an enthusiastic advocate for YouScreen since its early conceptualisation in 2018, I have no doubt this is fantastic news for thousands of women and people with a cervix who dread or put off going for the cervical screening appointment when it is due. Self-sampling puts women in control of their cervical screening, making it easier and more acceptable to them. We know from studies that there are many and varied reasons as to why women do not attend cervical screening. Believe it or not, one of the most common reasons is simply forgetting or delaying with every intention of making an appointment. For some, they fear the intimate physical examination, for others it is embarrassment, cultural, faith or religious reasons. For other women, they are too busy or distracted in their lives to make an appointment or have difficulty booking their appointment (Masset et al; Waller et al link; Marlow et al link).
Why is screening (and self-sampling) so important? What if I’ve already received the HPV vaccination?
Before you say this doesn’t affect me or I am vaccinated so I don’t need screening consider the following – over 3,000 women in the UK get cervical cancer each year (CRUK):
- Cervical cancer is 99% preventable through a combination of screening and vaccination
- Less than 1 in 100 (1%) women and people with a cervix will develop cervical cancer in their lifetime. If you have been vaccinated and do not attend for screening you are still at risk (link to cervical cancer information)
- Under- and un-screened women are at the highest risk of developing cervical cancer.
- In England, 56% of cervical cancers occur in under-screened women. By contrast, just 13% occur in women who are appropriately screened (and had normal test results).
- Compared with regularly screened women, unscreened women have up to 20 times the risk of advanced cervical cancer and three times the risk of micro-invasive cervical cancer, while infrequently screened women have 2-4 times the risk of regularly screened women (Landy et al 2016).
- Treatment for cervical cancer when found at an advanced stage can be very invasive and have a profound effect on quality of life (Living with cervical cancer).
Human Papilloma Virus
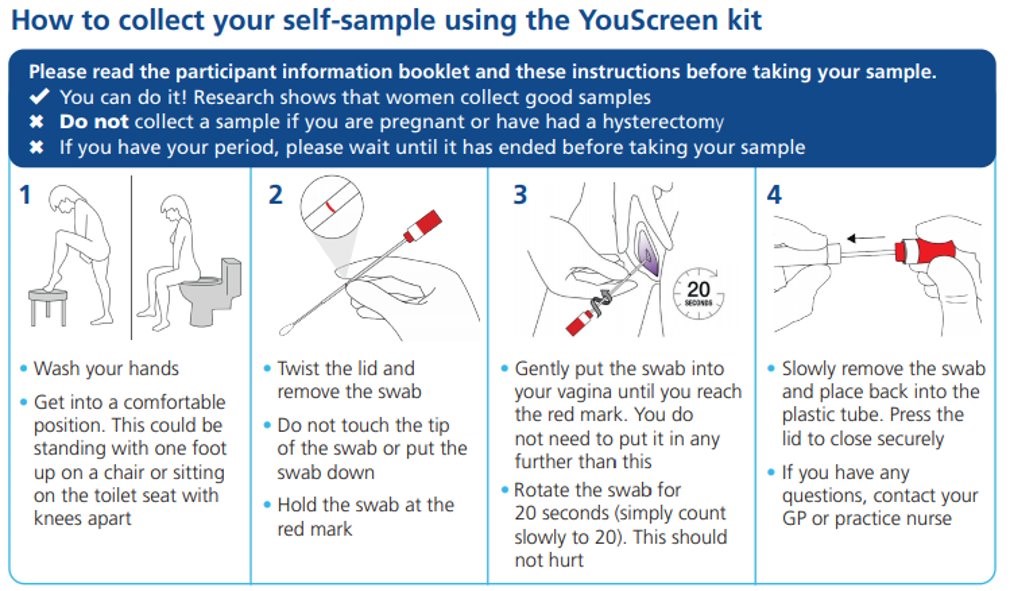
Though many of us still refer to the “smear test”, in reality, that is not what happens in cervical screening today. England introduced HPV Primary Screening in 2019. All samples are tested for HPV first. Only those samples where HPV is detected will have further cytology testing to identify if any abnormal cervical cells are present. It is because of HPV testing that self-sampling can be considered as a real possibility to be part of the future delivery of cervical screening. And the discomfort of the physical exam using a ‘speculum’ (the device used to hold the vaginal walls open), to view the cervix, and collecting cells from the cervix using a soft brush can be confined to follow up or when it is absolutely necessary rather than routine. If an HPV infection is present, HPV DNA can be found in the genital tract. Therefore, a woman can take the sample herself using a swab that looks like a long cotton bud. It is inserted into the vagina (no need to go as far as the cervix) and rotated gently for around 20 seconds. We know most women will take a great sample (of course we can!). The YouScreen Kit contains a pre-addressed and pre-paid envelope to return the sample to the lab. Easy. And the best news is that so far women are loving the offer, the GP practices are amazing and their enthusiasm is a reflection of how much they have struggled to reach women who do not attend their screening when invited. We hope women and people with a cervix will be enthusiastic in responding to the kits mailed out to them too.

By the time our eldest granddaughter reaches screening age, she will have had her HPV vaccination and will likely take her own cervical screening test every ten years. Maybe by then there will be a blood test, there will almost certainly be a urine test and if I am singing now I will be dancing with my walking frame then, knowing how much better an experience cervical screening will be; knowing that finally, cervical cancer will be a rare thing indeed.
More information about the YouScreen trial
The YouScreen trial will offer self-sampling kits to women who are overdue their cervical screening by at least six months in two different ways:
- via their GP when they attend for any reason other than a cervical screening appointment – we call this the opportunistic offer and
- via a direct mail out of an invitation letter and kit directly from the cervical screening programme – we call this the mail out offer
The trial is being delivered in 5 boroughs of north-central and northeast London. YouScreen is trying to reach women who do not attend regularly for screening as they are at the highest risk for developing cervical cancer. Over 30,000 self-sampling kits will be offered to eligible women during the year. The YouScreen study is led by Dr Anita Lim of King’s College London, commissioned by North Central London Cancer Alliance, in partnership with North East London Cancer Alliance. The study is run in collaboration with NHS England and NHS Improvement, Public Health England, NHS Digital and Jo’s Cervical Cancer Trust. The study is sponsored by UCL (University College London) and coordinated by the Cancer Research UK & King’s College London Cancer Prevention Trials Unit.
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.

