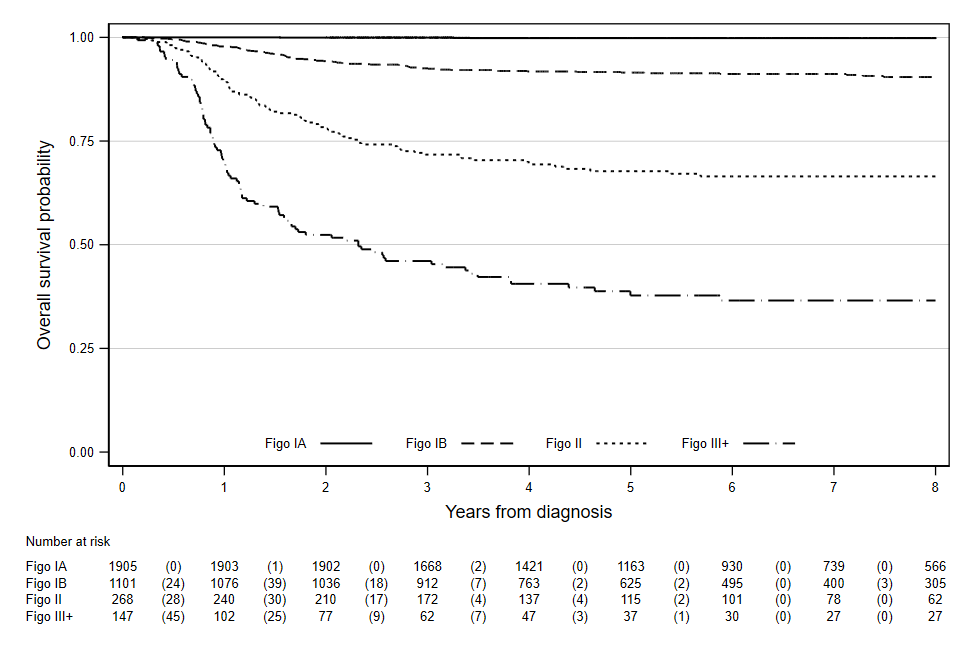
The earliest stage of cervical cancer (known as micro-invasive or stage IA) is treated with minimally-invasive fertility-preserving surgery, often as an outpatient. In fact, very often the treatment will be the same as that used to treat preinvasive lesions in the cervix. For the first time, we have shown that virtually no one died within 8 years of being diagnosed with stage IA cervical cancer aged 20 to 30 years: and the number of deaths was similar to that among (the same number of) women of the same age in the general population.
In this study, we observed three deaths among 1,905 women with cervical cancer aged 20-29y (observed survival 99.8%, 95%CI: 99.5-99.9%), whereas lifetables suggest 2.8 deaths were expected (relative survival 100%, 95%CI: 99.7-100%).
Diagnosis of micro-invasive cervical cancer certainly isn’t a death sentence. To the contrary – virtually all women are cured without the need for major surgery, radiotherapy or chemotherapy. Early-stage cervical cancer is asymptomatic hence screening is critical to ensure we detect and treat them before they progress to more advanced stages where treatment is more complex and outcomes less good.
The good news doesn’t end there, we also found that survival following a diagnosis of stage IB cervical cancer diagnosed through screening has better 5-year survival (94% survive) compared to IB cervical cancers diagnosed following symptoms (88% survive). So the early detection of 1B cervical cancer through screening halves the chances of it being fatal (from 12% to 6%).
Why these results are important.
In England, 62% of cervical cancers diagnosed at ages 20 to 29 are stage IA and a further 30% are stage IB.
The age at which women receive their first invitation to cervical screening in England has changed twice over the last 16 years. In 2004 it increased from 20 to 25 following evidence that screening at ages 20–24 provided little or no population benefit in terms of cancer prevention. In 2012, the age of sending out the first screening invitation was changed again; this time to 24.5 years. This was simply to enable women to be screened by their 25th birthday. Concerningly rates of cervical cancer in England at ages 25–29 increased from 10 per 100,000 in 2003 to over 20 per 100,000 in 2014. Further rates in women aged 20-24 increased from 2.7 in 2012 to 4.6 per 100,000 in 2014.
When we studied these increases in rates in detail we found evidence that screening is detecting early-stage cancers at age 24.5 rather than a little later at age 25. We also found that inviting women at age 25 years was associated with a substantial increase of cancers diagnosed at age 25 (of 44 per 100,000 women-years). These extra cancers were all stage IA or IB; no changes in the number of cancers diagnosed at more advanced stages (FIGO stage II+) was observed.
Screening saves lives. A diagnosis of early-stage cervical cancer is not a death sentence.
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.