A few weeks ago, on the 24th of February 2020, Michael Marmot released the newest review of his “Fair Society, Healthy Lives review”, detailing how socioeconomic inequalities in society (in terms of income, education and access to employment, for example) manifest as inequalities in health: impacting on life expectancy, years lived in good health (or QALYS), and infant mortality.
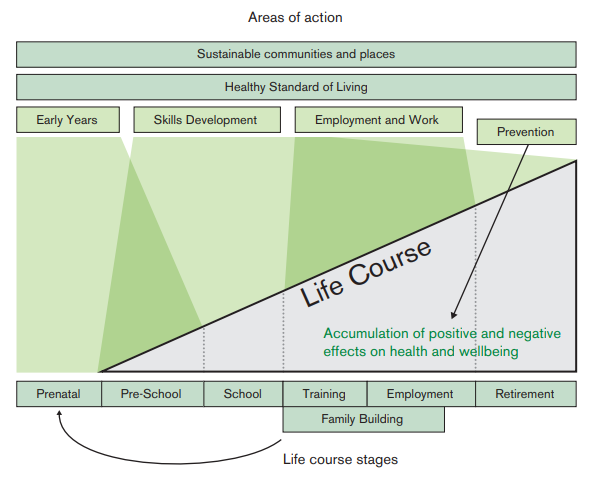
Marmot’s original review was pioneering in that it took a life-course focus to health, following how the health of an individual is impacted by inequalities at different stages of their life, as shown in the image below. This life-course approach has influenced many in the field of global health, making us think more about how the burden of disease (both communicable and non-communicable) is influenced by socioeconomic factors & environments across an individual’s life.
With that in mind, what are the key takeaways from the new review? More importantly, how can we apply what is in this new report to the issues we’ve seen in cancer screening and prevention?
The main points
One of the most shocking outcomes of the report is not only that life expectancy across the country has stalled, but life expectancy for those in the most deprived 10% of the population has declined. This decline is highest for populations in the North East areas of England, where areas of deprivation are most concentrated. This contrasts with London, which saw the biggest increases in life expectancy. In total, a woman living in the most deprived area of England can expect to live a total of 7.7 years less than someone living in a more well-off area; for men, this difference is 9.5 years.
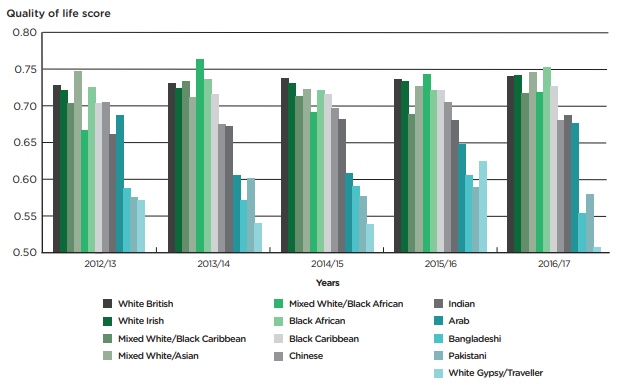
This difference in life expectancy is further exacerbated by ethnic background. Figure 2 shows how the most marginalised in society can expect to have a lower quality of life (Calculated via the EQ-5D, more detail here). This means that those from such ethnicities as Gypsy & Irish traveler, and to a lesser extent Bangladeshi, Pakistani or Irish not only have a lower life expectancy on average but can also expect to live more of their life in poor health (or DALY)
The report also stressed the importance of improving economic environments, particularly for those who are isolated or more distanced from the labour market. While wages have increased, the number of individuals who are working but still in poverty (earning below £15,000 per year) has increased. In addition, those in the 40% of lower earnings have seen their wages increase at a slower rate compared to the top 10% of earners, so this figure is likely to increase.
Health inequality & cancer
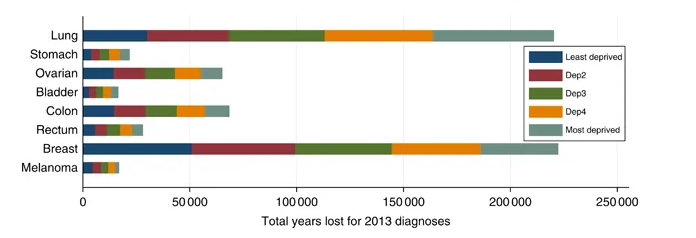
We know that existing inequalities in society can have big impacts on cancer outcomes. For example survival from cervical cancer decreases with socioeconomic status which is why it is sometimes referred to as a “disease of poverty”. Herein, inequalities relate both to the stratification of risk across a population, but also cancer outcomes after diagnosis. We know that smoking and obesity, both a risk factor for cancers, are more prevalent in deprived areas with higher socioeconomic inequality- increasing an individual’s risk of developing a number of cancers. In fact, it is estimated that the number of cancer cases in the UK attributable to smoking and obesity is 21%. With regards to cancer outcomes, evidence shows that those in the most deprived areas of England are more likely to have their cancer diagnosed at a late stage, compared to those in the least deprived areas. While the likelihood of survival for all cancers across all socioeconomic levels has increased over the last decade, the difference in survival between someone classified as ‘deprived’ versus someone classified as ‘affluent’ can be as much as 10%. This disparity in cancer outcomes, although not directly referenced in the Marmot report must play a role in the stagnation of life expectancy in the UK.
Participation in cancer screening has also been found to be related to socioeconomic status and ethnicity. For example, the most ethnically diverse areas are the least likely to respond to invitations to bowel cancer screening. The reasons for this non-attendance vary according to ethnic background. Health literacy tends to be lower in areas with more socioeconomic deprivation, in particular areas which are more ethnically diverse- meaning adherence both to screening programmes and to follow up procedures is lower than in more affluent & racially homogenous areas. Many older members of ethnic communities around England may speak English as a second language or not at all, making it difficult for them to engage with preventive services. Not responding to, or understanding these invitations increases the likelihood that cancers in these populations are diagnosed at a late stage, impacting on QALYs and life expectancy.
In the past, we’ve blogged about the relationship between structural racism & cancer outcomes. Herein, implicit bias may play a role in medical decisions- such as what treatment is offered or how much information on the available treatments is shared with the patient. This link between cancer and inequality isn’t so straight forward, however. Some cancers, such as breast cancers tend to be diagnosed more frequently in more affluent populations. Risk factors for breast cancer include not having children or having them later in life both of which are more common in developed countries.
Looking forward
The aim of Marmot’s report is not so much to point out political failings over the last 10 years but to illustrate how public health can work to reduce these issues over the next decade. The catch-all here is to not only improve equality in health but also to improve equity. The key, for instance, is to not only improve cervical screening coverage in more deprived areas but also to produce a programme that addresses the underlying issues for non-attendance- often socioeconomic in nature. While equity may be the solution here, achieving it requires a detailed understanding of the reasons behind the inequity, ensuring local councils, charities and organisations can work effectively to reduce it.
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.


Pingback: Building back better: How can cancer screening & prevention level up? – Cancer Prevention Group Blog