The HPV virus causes most cases of cervical cancer. This is why an HPV vaccination programme for girls aged 12 to 13 started in 2008.
Many people expected that cervical cancer rates in younger women would begin to fall soon after the introduction of HPV vaccination. Instead, rates have doubled. The number of women aged 20 to 24, who developed cervical cancer was 48 in 2012 but this increased to 82 in 2014.
Do you think this is worrying? We certainly did.
We were concerned as to why many more young women seemed to be developing cervical cancer and that it might be due to a failure in our public health strategy in the UK. One worry was that the increase in cervical cancer in women aged 20 to 24 was a result of not screening women in this age group. Another was that the vaccination was ineffective.
It was time to find out what was going on.
The NHS used to invite women for cervical screening from the age of 20, this changed to age 25 in England in around 2009. The change was made following the recommendations of the independent Advisory Committee on Cervical Screening. In December 2012 another change was made when the age of first invitation changed from 25 to 24.5. This was to try and ensure women attended for screening by their 25th birthday.
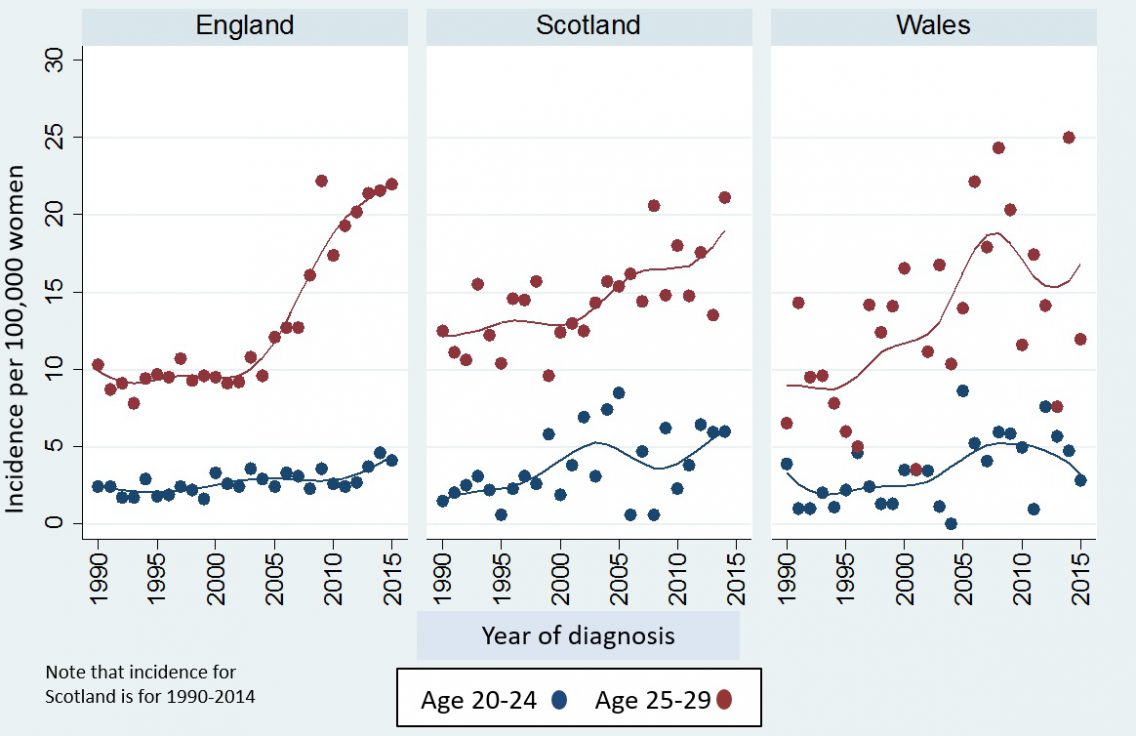
To see if the increase in cervical cancer was due to not inviting women aged 20-24 for screening, we compared rates of cervical cancer from 1990 to 2015 in women aged 20 to 30 in England with rates in Scotland and Wales (where they continued to offer screening from age 20 until after 2014). Although rates at ages 25 to 29 increased in all 3 countries, those in England saw the sharpest rise. Rates at ages 20 to 24 in England increased from 2013 onwards, which coincided with the change in the age at which the first invitation for screening goes out from 25.0 to 24.5.

Interestingly, despite there being no change in screening policy in Scotland, rates of cervical cancer at ages 20 to 24 in 2014 were as high as those in England. The increase in cervical cancer (in England, Scotland and Wales) under age 30 (even when screening is offered from age 20) is consistent with research suggesting that younger women are at a higher risk of HPV infection compared to older women.
Looking at the exact age at which cancers were diagnosed in England, we found that there was no increase in cervical cancer in women aged between 20 and 24.5. The increase was limited to the six months after the screening invitation was sent out at 24.5 We also saw that there were fewer cancers diagnosed in the six months after a woman’s 25th birthday than there had been when invitations were sent out on the birthday. This suggests that because women were coming for screening that bit earlier, cervical cancers were being picked at age 24 that would previously have been found at age 25.
When we looked at if/how far the cancers had spread, we found that the additional cancer diagnoses were all early stage. There was no increase in cancers that had spread beyond the cervix. Most women with early stage cervical cancer diagnosis will make a full recovery and most can be cured without affecting their ability to have children.
We also found that not inviting women for a screening test under age 25 resulted in an increase in the number of cancers diagnosed at age 25 and at 28. The biggest increase was in the six months after the 25th birthday. Again, the increase was restricted to early stage cancer. An increased detection of cancer cases is expected when screening is first introduced, so these results are not surprising. The increase at age 28 most likely reflects screen-detected cancer in women responding to their second screening invitation sent on their 28th birthday.
In conclusion, there is no evidence that changing the cervical screening starting age has led to more women getting cervical cancer. Rather, screening is detecting early stage cancers at age 24.5 rather than a little later at age 25.
We think it’s too early to draw conclusions regarding the effect of vaccination on cervical cancer. It was only from March 2016 that women vaccinated in the last year of school would have been invited for screening. The first women vaccinated (in 2008) would have been aged 23 to 25 in 2015 (the most recent year for which cancer incidence data exists in our study). Few women develop cancer within 8 years of an HPV infection. So, women aged 23-25 with cervical cancer who were vaccinated at age 16-18 would most likely have been infected with HPV before they received the vaccine.
Click here to read the full paper.
To ensure women minimise their risk of cervical cancer, we urge them to take advantage of their invitation even if they think they are at low risk.
If you have any questions about cervical screening, speak to your GP or practice nurse. You can also find lots of information on NHS Choices.
You may be interested in the following related content: Cervical cancer: the epidemic that never was!
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.

Pingback: Stage 0, 1, 2, 3, 4 Cervical Cancer: Treatment Options and Survival Rate
Pingback: Over 99.5% of young women survive following a diagnosis of IA cervical cancer – Cancer Prevention Group Blog